Sexual health
STI vs. STD: What’s the Difference Between a Sexually Transmitted Infection and a Sexually Transmitted Disease?
What we do while close up and personal can sometimes result in pervasive yet preventable medical conditions that require treatment ASAP. These are conditions you can catch while engaged in some form of sexual behavior.
Once called “social diseases,” or labelled with offensive slang terms, sexually transmitted infections (STIs) and sexually transmitted diseases (STDs) and their symptoms have often been a source of shame and misinformation. Fortunately, it’s now easier than ever to obtain good, clear information.
This article will get you started.
STI vs. STD: What's the difference?
You've probably heard the terms “STI” and “STD," and you might have wondered if they're the same thing or if there's a difference between an STI and an STD. Let's start by clearing this up.
The acronym “STI” stands for “Sexually Transmitted Infection” and “STD” stands for “Sexually Transmitted Disease.” Though these terms are often used interchangeably, this isn’t quite accurate.
STI and STD do refer to the same set of infections passed from one person to another primarily through sexual contact and that might progress to a disease state. These include diseases such as gonorrhea, chlamydia, syphilis, HIV/AIDS, herpes, and others. However, each term refers to a different stage of an infection with one of these diseases.
The Shift from STD to STI
An infection (STI) may not always progress to a full-blown disease, especially if the infection is treated promptly. However, when an infection progresses, with or without treatment, it becomes a disease state. This is the main clinical distinction between the two terms. It’s important to remember though that not all infections — or diseases — will result in detectable symptoms.
There’s also the nuanced distinction of “infection” having less of a stigma than the term “disease.” This is the reason why most medical professional use the term STI instead of STD most of the time. When it comes to sexual health and treatment of STIs and STDs, reducing stigma and shame is of the utmost importance.
Breaking the Stigma
Sadly, sexual behavior itself is often still stigmatized and that stigma increases for people who catch an STI. But STI cases are very common and on the rise in the U.S. In 2018, estimates showed that one in five people in the U.S. have an STI, approximately 68 million infections. In 2024, the World Health Organization also raised the alarm on STI increases.
There is no reason to be ashamed or embarrassed about contracting an STI. Having an STI is not a reflection of character. The most important thing is to get tested, get a medical diagnosis, be honest with your partner(s) about your results, and get treatment! Most STIs and STDs are quite treatable. And preventable!
A number of STIs must be reported, by law. If you test positive for chlamydia, gonorrhea, hepatitis B and C, neonatal herpes, HIV, and syphilis, you must notify your current and previous sexual partners within one business day so that they too may get treatment. In the case of neonatal herpes, the infant’s medical provider will probably already know.
Common STIs & Their Treatments
STIs are caused by bacteria, viruses, or parasites. The CDC says that of the eight most common STIs, four are “easily treated and cured if diagnosed early: chlamydia, gonorrhea, syphilis, and trichomoniasis.” The other four — all viruses — can become serious if not diagnosed and treated.
Bacterial STIs — such as gonorrhea, syphilis, and chlamydia — are treated with oral or injected antibiotics. The viral STIs — human immunodeficiency virus (HIV), human papillomavirus (HPV), herpes simplex virus type 2 (HSV-2), and hepatitis B virus (HBV) — are treated with oral antiviral or antiretroviral medications. There is no cure. These STIs require ongoing management.
Trichomoniasis is caused by a parasite and is usually treated by either Metronidazole or Tinidazole.
Prevention is Essential
STIs are preventable! So, what you need as a responsible sexually active person is a prevention strategy!
First, you’ll want to learn about STIs so you know what they are, their symptoms, tests, and treatments, whether it's common to be asymptomatic and still have the the STI, and the best means of protection from each STI.
Because early detection is the key to preventing complications, make regular STI testing a part of your overall health regimen. The CDC has a range of screening recommendations based on the specific STI, your age, gender, and other factors, like whether you have multiple partners or have unprotected sex. You can check those here and expect your medical provider to adhere to them.
In general, you might want to plan on an array of tests every six months or once a year, in addition to before and after engaging with a new sex partner. And definitely test immediately if you experience any symptoms!
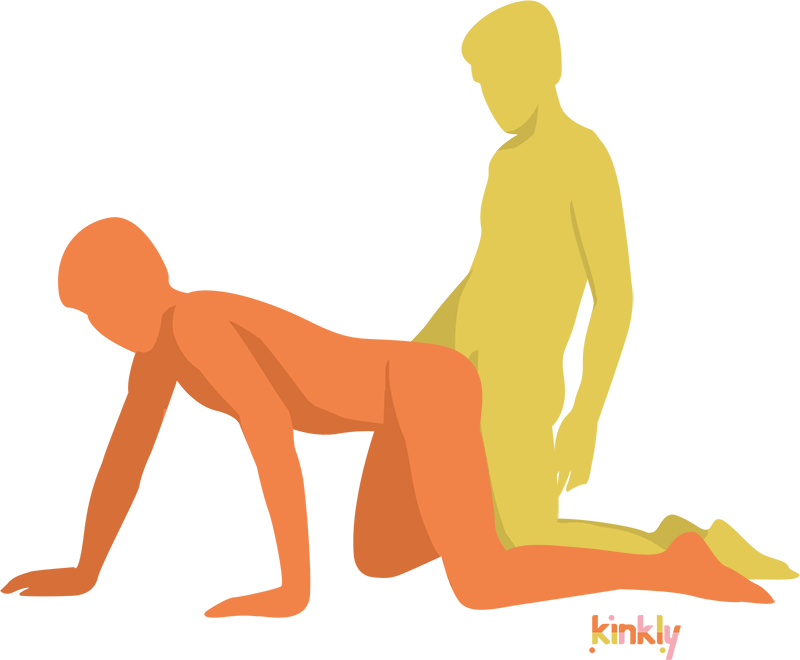
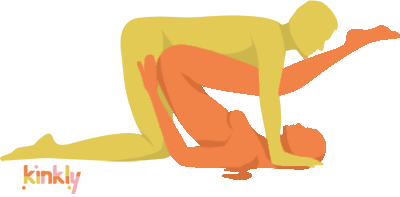
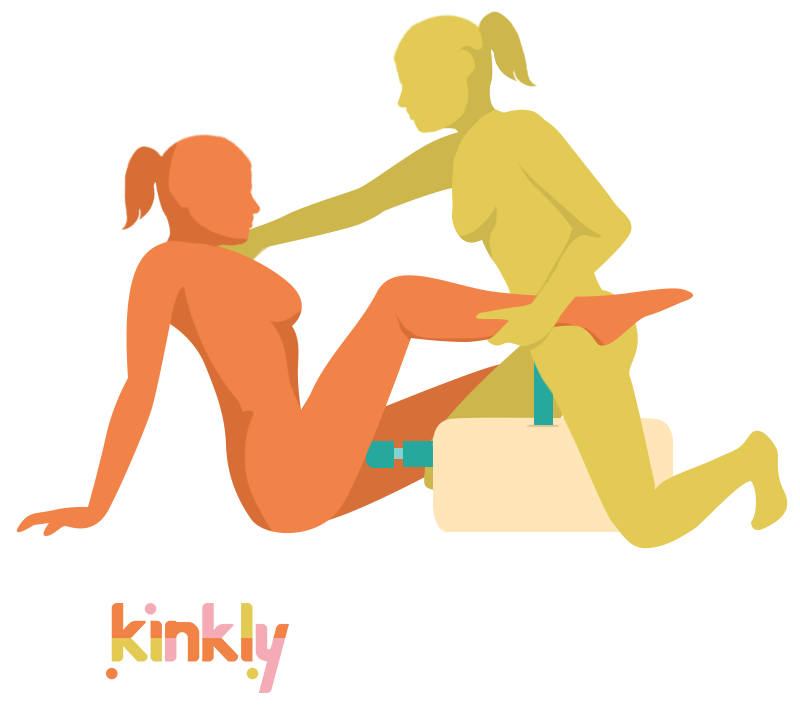
Then there’s safer sex practices! Get familiar with barrier methods for vaginal, anal, and oral sex, and other activities that include sharing sexual fluids, such as genital-to-genital contact and sharing sex toys. Barrier methods include condoms, internal condoms (sometimes called “female condoms”), dental dams, and gloves and finger cots made of latex, nitrile, or vinyl. The more comfortable you are with these options, the easier it will be to make safer sex, sexy.
HPV, chlamydia, syphilis, and gonorrhea can be found on sex toys too. So, always clean them, both before and after use, with warm water and antibacterial soap, according to the product directions. Let them dry well before storing.
Then make sure you store them in their original package, a pouch, or any other container that will keep your toys away from dust and contact with other toys. And while you’re at it, wash the outside of that lube bottle too!
The Bottom Line
Exposure to STIs and practicing prevention are a normal part of navigating our sex lives and preserving sexual health. You’re not alone in this and neither are your partners. But the more proactive you are with testing and prevention, the better off you are.
It’s up to you to learn as much as you can so you can take charge of your sexual health. With honest communication, regular testing, and consistent safer sex practices, you will be far better off, even if you do contract an STI at some point. You’ll be more likely to get the help you need before the STI progresses to an STD.
They’re certainly inconvenient, and not ever any fun, but there’s no shame in contracting an STI — ever.