Let’s talk about an important but often overlooked condition: pelvic inflammatory disease (PID). If left untreated, PID can cause chronic pain and infertility. That said, PID is curable if treated promptly. This article covers everything you need to know.
What is Pelvic Inflammatory Disease (PID)?
Pelvic inflammatory disease is a medical condition that affects the female reproductive system. It can cause various symptoms, including pain and inflammation in the pelvic region.
“The pain can be felt deep inside your pelvis or can include pain with sex and urinating,” says Christine Greves, MD, an OB-GYN and medical contributor for Drugwatch.
PID is often a complication of an untreated sexually transmitted disease (STD), like chlamydia or gonorrhea. It develops when bacteria from the vagina spread to other reproductive organs like the ovaries, fallopian tubes, and uterus. PID can also develop without an STD if the bacteria that’s in your vagina travels into your reproductive organs, notes Dr. Greves.
“Douching can increase that risk,” she adds.
Fortunately, PID is curable with antibiotics. However, the damage PID causes in the uterus and fallopian tubes may be irreversible, leading to infertility. This is why early detection and treatment of PID is so important.
It’s best to see a doctor if you have any signs of a pelvic infection.
Symptoms of PID
So, what are the signs of a pelvic infection? Well, sometimes, it can be really hard to tell. Not only do symptoms of pelvic inflammatory disease range from mild to severe, but they can also be vague and mimic other conditions. In fact, some people with PID don’t experience symptoms at all.
The most common PID symptoms include:
- Pelvic inflammation and pain
- Vaginal discharge and stomach pain
- Fallopian tube pain
- Painful or irregular periods
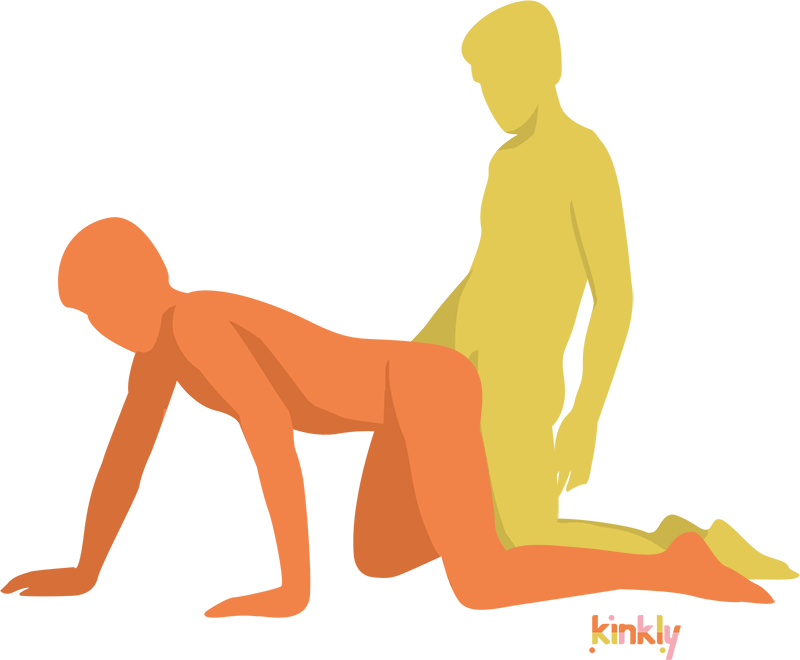
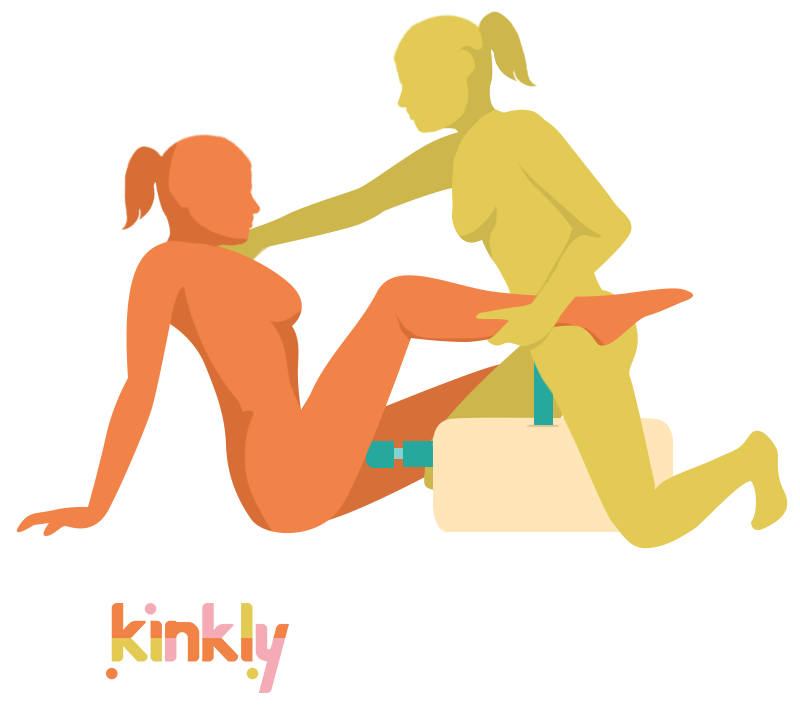
- Pain during sex
- Fever
- Nausea or vomiting
You should consult a healthcare provider if you have any signs and symptoms of pelvic inflammatory disease. Getting prompt treatment can prevent long-term pain and unwanted health complications.
Causes and Risk Factors for PID
What causes pelvic inflammatory disease? In 85% of cases, it’s due to complications of an untreated STI, but there are other factors, too.
Here are some common risk factors for PID:
- A new sexual partner or multiple sexual partners
- Bacterial vaginosis
- Unprotected sex
- Previous history of PID
- Previous STIs
- Having an intrauterine device (IUD) inserted
- Tubal ligation
- Age
- Recent childbirth or abortion
Read More: Is This Gonorrhea? Here’s How to Tell if You Have This Common STI
Possible Complications of PID
Most people who treat their PID with antibiotics have a full recovery and don’t experience any long-term issues. That said, PID can cause serious and long-term complications if not treated quickly.
These complications may include the following:
- Repeated PID episodes
- Chronic pelvic pain
- Scarring of fallopian tubes
- Ectopic pregnancy
- Infertility
- Formation of abscesses
Diagnosis and Treatment of PID
To get an accurate diagnosis and the correct treatment, it's essential to see a healthcare provider as soon as you have any symptoms that indicate PID. Here's what to expect at your appointment.
How is PID diagnosed?
A healthcare provider can usually diagnose PID through a pelvic exam. Sometimes, an ultrasound and additional testing are needed. In some cases, your healthcare provider may perform an endometrial biopsy by laparoscopy, which involves inserting a small camera through a cut in your belly button to examine the reproductive organs, and taking a small tissue sample from the uterus.
Your provider will probably test you for STIs like chlamydia and gonorrhea as well, since they often cause PID.
Treatment options
Pelvic inflammatory disease treatments typically involve antibiotics. Until you finish your course of treatment, it’s best to avoid sex, douching, or tampons and wait for a doctor’s approval to resume.
You should also notify sexual partners of your diagnosis and have them get tested for STIs, even if they feel okay. It’s important to note that you can get reinfected if your partner has an active STI.
In severe cases, PID can cause health complications that require hospitalization. While rare, surgery may be needed to repair or remove parts of your reproductive organs.
Prevention of PID
The best way to reduce your risk of PID is by being proactive about your health. Get annual checkups and regular STD testing to prevent infections from flying under the radar. If you do have an STD, seek treatment promptly to reduce your risk of developing PID.
Read More: STI vs. STD: What’s the Difference Between a Sexually Transmitted Infection and a Sexually Transmitted Disease?
When to See a Doctor
It's best to see a doctor if you’re experiencing any symptoms of PID.
“See your doctor if you have pain, discharge, or any concerns,” Dr. Greves says. “If it is affecting your quality of life, and if you think something could be wrong, seek medical attention, especially if you have a new sexual partner or have had a recent medical procedure.”
A healthcare provider can diagnose you and get you started with antibiotic treatment.
The Bottom Line
PID can cause painful and disruptive symptoms, but treatment is available, and recovery is possible. Getting an early diagnosis and treatment is important to manage your symptoms and prevent further complications.
As intimidating as doctors can be, it’s important to be open about your health so they can offer sound medical advice that can improve your overall health and well-being.